
HUNTINGTON WOODS, Michigan – For years, retired Wayne State physics professor Talbert Stein, B.A. ’62 enjoyed brisk walks through his picturesque neighborhood and occasional hikes in some of the nation’s most breathtaking national parks.
“Throughout my life, I was just in love with walking and hiking,” Stein said. “I’ve done a lot of mountain hiking; it’s one of my favorite things, especially getting up so high you can get the panoramic views from above the timber line.”
But it was Stein’s passion that set off internal alarm bells while visiting family in Pennsylvania in 2015. While on a vigorous walk, an excruciating pain in his right calf nearly brought him to his knees.
“I was taking one of my usual long walks with my sister-in-law,” said Stein, who taught at WSU for 33 years. “She’s a marathoner, so walking with her was something I enjoyed. But for the first time in my life, there was a complete showstopper.”

Concerned by the sudden acute pain, Stein had to rest a bit before continuing on the trail. A short distance later, the debilitating pain returned.
“It was very disturbing to me because everything always worked smoothly and painlessly prior to that,” the 81-year-old Stein recently said.
Once home, Stein — a self-described tinkerer and problem-solver — pored over medical journals seeking an explanation. He quickly diagnosed the symptoms as peripheral artery disease (PAD), which is the narrowing or blockage of the vessels that carry blood from the heart to the lower extremities. A subsequent visit to a vascular surgeon confirmed that Stein had a blockage in the superficial femoral artery.
According to the Centers for Disease Control and Prevention, PAD effects approximately 6.5 million Americans age 40 and older. People over 60 are at greater risk of contracting the disease, which could lead to heart attack or stroke.
Understandably, the diagnosis was troubling.
“It was deeply disturbing to me because walking is one of my great passions,” he said. “As you get older, maybe some people are OK with losing abilities, but I’m not one of those people. I feel these physical abilities are all precious. There’s not one that I would willingly give up.”
Another passion for Stein is playing fiddle. Since retiring, he has played with a local trio, playing gigs around town, but PAD has temporarily stopped the music.
“I’m still invited to play with them,” Stein said, “it’s just I basically told my compatriots that I need to focus on this (PAD) and try to get myself out of trouble. But fiddle is still a big part of my life.”
Armed with his diagnosis, Stein, who’s been physically active since he was a student at Detroit’s Cass Technical High School, was ready to conquer the disease. “So, I started to begin battling the whole thing of aging,” he added.
But for Stein, a lifelong learner, just knowing the root of the pain wasn’t comfort enough. After all, he’s used to collecting and analyzing data to solve problems.
“I was exquisitely tuned in to how my body felt when things weren’t working well,” he said. “Part of the thing with me is when things stop working, whether it’s the car or an appliance in the house — for example, the furnace stops working on the coldest day of the year — I love to get in and repair it myself. So, when this right leg stopped working, it was a natural thing for me to think, ‘Is there something I can do?’
“For me, when something stops working, it’s like someone is giving me an invitation to a party — literally. There’s part of me that gets excited when something goes wrong because I think in my mind it’s an opportunity to learn.”
A plan of attack
With the advice of his vascular surgeon, WSU alumnus Dr. Paul Bove, Stein went to work on reversing the effects of atherosclerosis in the superficial femoral artery.
“One of the key aspects to vascular care, and medical care in general, is self-awareness, being aware of those factors that affect a patient’s medical condition,” Bove said. “Dr. Stein had incredible insight into those factors that allowed him to walk further. When patients understand this and can implement change, whether it is in their activity, as in Dr. Stein’s case, or other aspects of their lifestyle, for example plant-based or Mediterranean-style diets and smoking cessation, that is when you get the best results.”
Stein began a regimen that included fasting before morning walks. He also used a recumbent stationary bike on the days he didn’t walk. Stein credits the bike’s resistance on his quadriceps to deliver more oxygenated blood to the calf muscles.
“When I didn’t eat prior to walking, say I had eaten the prior evening and I took my walk the following morning on a 10-hour fast, those were by far my best walks,” Stein said. “It was correlated.”
For about a year, Stein said things worked out somewhat, but not in an exciting way. He reached a plateau and started heading downward, subjectively. “I was doing worse and heading into trouble again, in spite of following the protocol and the medical journals,” Stein said.
Stein’s pain reached a level that was affected even the simplest of daily chores.
“It got so bad that I would actually go to a grocery store with an adjacent parking lot and I would start to walk to the store — less than 50 yards away — and the pain would get so bad that it would stop me halfway,” he said. “I didn’t feel like walking around that market and I would head home.”
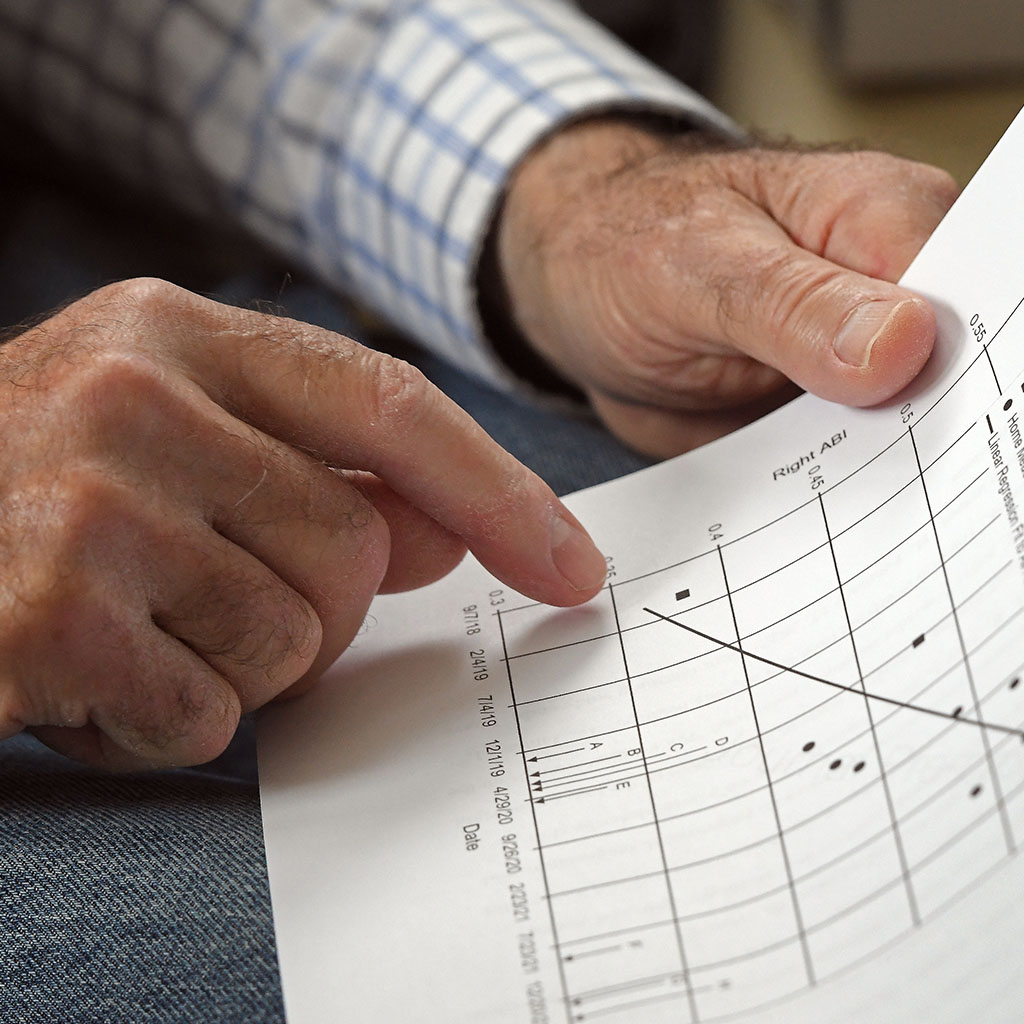
Stein decided to quantify his progress to see what was really happening, because from day to day and from hour to hour, there could be dramatic changes in his walking. It could feel better or it could feel incredibly worse.
“I had an iPhone with a clock app and in the app you can enter laps,” Stein said. “So, what I started doing, which is natural to me, is quantifying my walking.”
His data collection began with measuring two data points: walking times and resting times when pain was present.
“I treated the data as an experiment,” Stein said. “I began quantifying everything. When I got home, I would enter all of that data in the spreadsheet. I would find out all sorts of things that were of interest to me, such as, what was the average speed of a walk? How much of that total time did I spend resting? I even devised a figure of merit for my walking. So, I came up with a number and a little formula for that.”
But then came the PAD complications. In 2020, Stein was diagnosed with critical limb ischemia (CLI), a condition common to PAD patients, which caused open sores on the tips of Stein’s toes. The ulcerations didn’t heal and the tissue started to turn black.
“When you see your tissue turning black, you think gangrene,” Stein said. “My thought was, ‘This is heading south, and if I don’t get on it, I’m looking at amputation.’”
Pitching to medical journals
Stein found that when he didn’t fast prior to exercising, his walks were much shorter and more painful.
“When you eat, the most important thing the body is focused on is digesting that food and getting the nutrition and everything that is associated with that, which is essential,” Stein said. “So, it dilates arteries going to the digestive tract, and that correspondingly closes down some arteries in other places. So, for me, it pushes me completely into a ditch. If I don’t eat and I don’t divert blood to the digestive tract, then there is more blood available to give to the starving muscle in my calf when I’m walking.”
Stein continues his routine, fasting for 10 hours before long walks or hikes and riding the recumbent bike on days he’s not pounding the pavement.
“By dialing in as much resistance as I wanted, I didn’t get pain in my calf, but I got pain in my thigh,” Stein said of the bike. “I was stressing my quads more than the calf muscle when I biked and stressing the calf muscles more than my quads when I walked. That was as interesting piece of information. Using the bike on the days that I wasn’t walking, my walking was becoming better and easier.”
But once stricken with CLI, Stein had to consider new steps. That’s when he took to the stairs in his home.
“I knew I could cause more stress on my quads if I lifted my entire bodyweight up the stairs,” said Stein, who retired from Wayne’s College of Liberal Arts and Sciences in 2004. “What could be better than that for an 80-year-old person? Normally, I climb two, three, four sets of stairs a day. Now, I figured I would start out doing 14 flights of stairs a day. I did it barefoot because these wounds were getting into everything.”
Although Stein often begins his stair climbing with some typical aches and pains in joints and muscles, they gradually disappear completely after climbing several flights. If pains worsen, he backs off until they’ve resolved, and resumes climbing after some time passes.
Stein increased his average daily flights to 30, and his average daily time spent climbing was 12 minutes. Over the course of his two-year long stairclimbing study, he’s ascended 22,185 flights – the equivalent of 42 miles, or more than seven trips to the top of Mt. Everest.
In February 2018, Stein had a setback, fracturing a hip in a bad fall. He underwent surgery to insert a titanium rod along the femur. But once fully recovered from hip surgery, Stein returned to stair climbing to continue his battle against PAD and CLI.

“I got on those stairs and started climbing. I committed to it,” he said. “The thing associated with this problem is the tissue is starving for oxygen and nutrition, and you get this neuropathy, horrible pain in your feet. People with PAD talk about it all the time. The pain was incredible.
“I literally would get into bed, pull a bed sheet over me, and the bed sheet contacting those toes hurt like hell. I could hardly believe the pain.”
Today, Stein feels much better, and his cardiologist is impressed.
“He has told me that he tells his other patients what I do,” Stein said. “He feels what I’m doing for me is better than what he has to offer me surgically. He’s never suggested that he would intervene surgically, and my attitude is that surgery is a last resort.”
Throughout his illustrious career, the retired physics professor had hundreds of scholarly papers published in scientific journals, but never in a medical journal — that is, until the research paper on his single-patient case study was accepted and published by the Annals of Vascular Surgery. It’s highly unusual for peer-review medical journals to publish research performed by non-physicians. It’s also uncommon for journals to accept single-patient case studies, especially from someone who’s done a study on themselves, which is subject to more possible bias.
“The recumbent bike and stair climbing became important things,” Stein said. “Together, with the recumbent bike and the fasting, that was the essence of the first paper.”
Stein had a subsequent paper published by The Journal of Vascular Surgery Cases, Innovations, and Techniques.
Stein is humbled that the journal reviewers took interest in his submissions.
“I’m a patient off the street and I don’t know anything about this except I’ve dug into it since I got the problem,” he said. “For them to pay attention to me and send it out for review, that’s a huge step. I’m completely lucky that I got an editor who read this thing and thought maybe there’s some merit to this thing even though I’m not a physician.”
But now what?
Stein says he hopes someone in the medical research field will find the value in conducting a clinical trial. He would like to see someone sufficiently interested take his research further and do a clinical trial involving 50 to 200 patients.
“I think this needs to be tested with many patients in order to see if it has efficacy for other patients,” Stein said. “My first hope is that this will stimulate that kind of thing in a multi-patient test.”
