A Wayne State University School of Medicine oncologist and physician scientist has received a significant gift from a dedicated donor to promote his research.
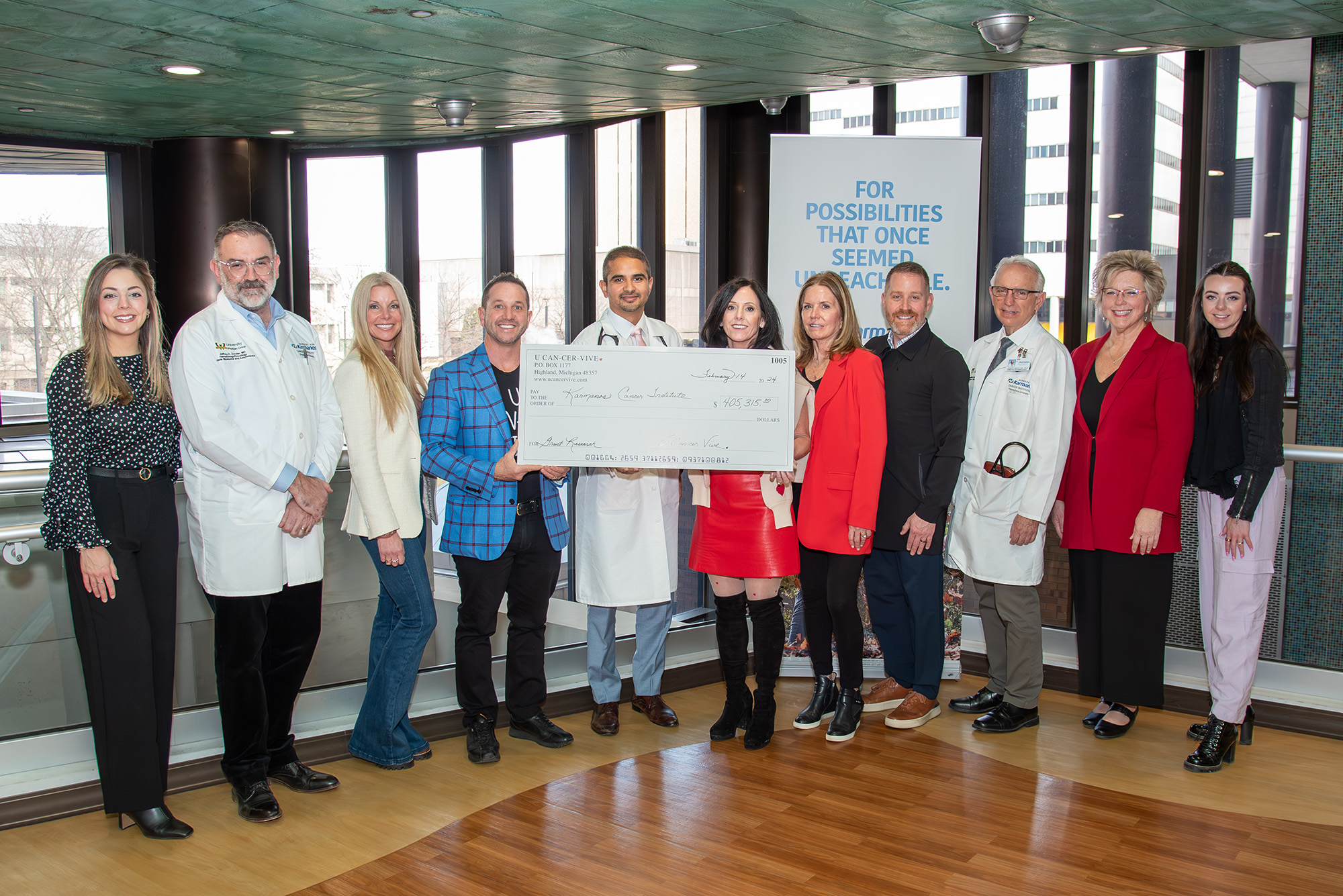
The U CAN-CER-VIVE Foundation awarded Suresh Balasubramanian, M.D., assistant professor of Oncology and a member of the Hematology Oncology and Multiple Myeloma and Amyloidosis Multidisciplinary teams at the Barbara Ann Karmanos Cancer Institute, and his team of investigators a $405,315 grant for their research, titled “Biological Aging and Mutational/Immunological Signatures as Prognostic and Predictive Biomarkers for Treatment of Hematological Malignancies.”
“Receiving such generous backing from the U CAN-CER VIVE foundation is truly significant. Their consistent support for Michigan Researchers over the past several years has been instrumental in advancing scientific research,” Dr. Balasubramanian said. “This grant will enable us to employ the latest scientific techniques to finetune and validate a new biomarker in different clinical settings, which has the potential to transform the care of our patients.”
Dr. Balasubramanian is a hematologist and medical oncologist specializing in the treatment of clonal hematopoiesis, myelodysplasia, leukemia, lymphoma, and multiple myeloma. He and his team are exploring the idea of estimating biological age as a better surrogate to determine treatment decisions for certain cancers as opposed to chronological age. Chronological age measures the number of birthdays a patient has, whereas biological age would help consider changes that happen in a patient’s body at the level of cells and their components.
“Changes at the cellular level can be DNA damage, cells getting old and stopping to divide, adjustments to how genes work that don’t involve changes in the actual DNA code, cells losing their ability to produce energy efficiently, and changes in how our immune system works and how our body handles energy and nutrition as we get older. Many of these changes can make a person susceptible to cancer,” Dr. Balasubramanian explained.
His team is specifically looking at DNA methylation, a small chemical modification that occurs in DNA. Dr. Balasubramanian said these changes are predictable as we age and can be measured using advanced machine-learning tools to estimate their biological age.
“In our study presented at the American Society of Hematology meeting in December 2023, it was demonstrated how biological age differences from one’s chronological age (epigenetic age acceleration) could influence treatment response,” he said. “We plan to study this biological age and epigenetic age acceleration further in unique clinical settings, like how biological age would influence the outcomes in allogenic transplant recipient patients and various myeloid malignancies and be used as a biomarker for response in a multiple myeloma clinical trial. Additionally, we are also looking at whether biological age has any role in the racial disparity of cancer outcomes.
“We also envision incorporating biological age as a standard of care for cancer treatment,” he continued. “In the future, we expect to expand the input into the machine-learning tool to include additional aspects of cellular aging, not limited to just DNA methylation, to estimate the biological age.”
Dr. Balasubramanian is collaborating on this research with co-investigators Joseph Uberti, M.D., Ph.D., hematologist and medical oncologist, Bone Marrow and Stem Cell Transplant MDT leader, and Tumor Biology and Microenvironment Research Program member, and Jeffrey Zonder, M.D., hematologist, Multiple Myeloma and Amyloidosis MDT leader, Hematology Oncology MDT member and MT Research Program member.