
The National Institute on Minority Health and Health Disparities has awarded Wayne State University $18.15 million over five years to establish a Center for Multiple Chronic Diseases Associated with Health Disparities: Prevention, Treatment, and Management that will use community-based interventions deployed from three research institutions to fight hypertension, heart failure and coronary heart disease in the Black population.
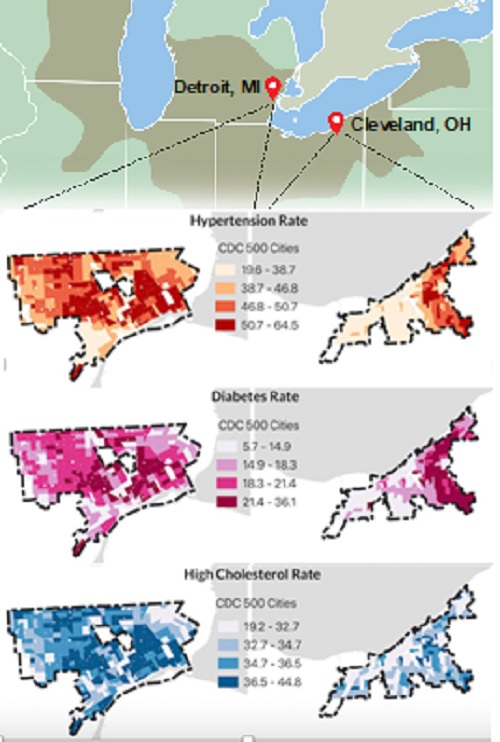
The Addressing Cardiometabolic Health Inequities by Early PreVEntion in the GREAT LakEs Region, or ACHIEVE GREATER, Center is a proactive versus reactive approach to reducing overwhelming cardiometabolic health disparities and downstream Black-White lifespan inequality in Detroit and Cleveland, two uniquely comparable cities.
Building upon existing collaboration and resources across Wayne State University/Wayne Health, and the Henry Ford Health System in Detroit, and Case Western Reserve University/University Hospitals in Cleveland, ACHIEVE GREATER will include three distinct but related projects that focus on interrupting early stages of pathogenesis by addressing multiple domains of influence that contribute to disparate health outcomes in the Black population, specifically biological, behavioral, physical/built environment, sociocultural environment and the health care system.
The overarching goal is to mitigate health disparities in risk factor control for chronic conditions of tremendous public health importance, which drive downstream lifespan inequality, said ACHIEVE GREATER principal investigator Phillip Levy, M.D., M.P.H., the Edward S. Thomas Endowed Professor of Emergency Medicine and assistant vice president of Translational Research for WSU, as well as Chief Innovation Officer of Wayne Health.
A core component of ACHIEVE GREATER is the use of collaborative care involving community health workers and pharmacists, to deliver a pragmatic, personalized, adaptable approach to lifestyle and life circumstance intervention, called PAL2. Community health workers serve as a liaison between the patient and health care providers, and have often shared the lived experience of the person they’re trying to help. They know the local resources and can help fill gaps in social knowledge.
“The future of medicine is community health workers engaging people where they live, work or play to enhance access to not only medical care, but social services, to improve their health outcomes,” Dr. Levy said. “How do we help people with challenging life circumstances so their lifestyle can improve? Health care has to exist beyond the four walls of a doctor’s office. Let’s get you the person who is going to help you with your needs.”
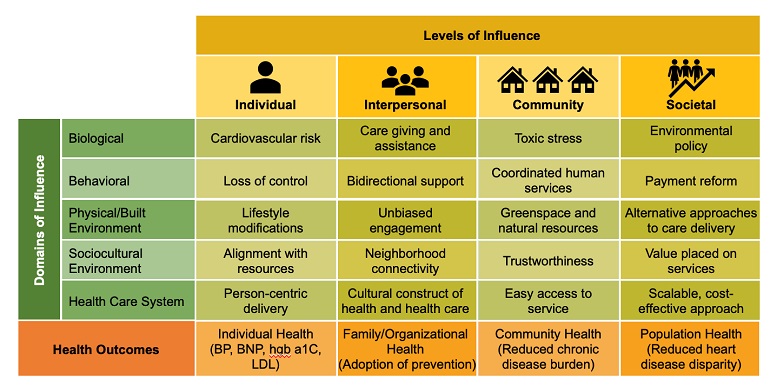
The ACHIEVE GREATER center seeks to improve lifespan equality by implementing the PAL2 intervention to address multi-level risk profiles in Black patients with cardiometabolic risk factors who live in racially concentrated areas of poverty; and use the Practical Robust Implementation and Sustainability Model to assess program reach, effectiveness, adoption, implementation and maintenance, or RE-AIM. It will also profile the incidence density of chronic hypertension, heart failure and coronary heart disease in electronic health records, and interrogate multi-level risk profiles by probing interrelationships among geospatial factors, including aspects of the built environment, person-level socio-behavioral factors and clinical characteristics. In addition, early-career scientists will be trained to focus on mitigating the chronic hypertension, heart failure and coronary heart disease disparities that drive downstream lifespan inequality and disseminate key information uncovered during the project’s trajectory to policy makers, payers, public health departments and other stakeholders to drive sustainable change.
Overall U.S. life expectancy stalled before the COVID-19 pandemic, according to the 2018 article, “Trends in health inequalities in 27 European countries,” published in Proceedings of the National Academy of Sciences, largely because of midlife mortality from cardiovascular diseases. “Life Expectancy and Mortality Rates in the United States, 1959-2017,” from the Journal of the American Medical Association, showed age-adjusted midlife mortality rates for hypertensive diseases and obesity increased respectively by 79% and 114% from 1999 to 2017. People from areas with increased vulnerability related to socioeconomic status died more often and younger than people from less disadvantaged areas, according to two recent studies published in the American Journal of Public Health and JAMA Internal Medicine.
COVID-19 exacerbated an already worsening situation, and the U.S. Black-White life expectancy gap increased by 40% in the first eight months of 2020, a 2021 study published in the Proceedings of the National Academy of Sciences showed.
Dr. Levy launched in 2019 a precision approach to population health, known as the Population Health OutcomEs aNd Information Exchange, or PHOENIX. The novel geocoded system uses de-identified electronic health records and information on population-level social determinants to paint an overall picture of health in Michigan area by area, using color-coding to graphically display differences.
“When COVID hit, we were very well-prepared to leverage PHOENIX for COVID. In my mind, PHOENIX was always leading to (ACHIEVE GREATER),” Dr. Levy said.
He also leads Wayne State’s new, nearly $2.64 million, four-year project, that began Oct. 1, titled Linkage, Empowerment and Access to Prevent Hypertension, or LEAP-HTN, funded by the American Heart Association as part of the $20 million RESTORE (Addressing Social Determinants to Prevent Hypertension) Health Equity Research Network.
Each ACHIEVE GREATER primary project will be led by a principal investigator from one of the three participating institutions. All three will be supported by an administrative core led by Dr. Levy; a community engagement core, co-led by WSU Professor of Family Medicine Deborah Ellis, Ph.D., Assistant Professor of Family Medicine and Public Health Sciences, Division of Behavioral Sciences Elizabeth Towner, Ph.D., and WSU Assistant Professor of Family Medicine and Public Health Sciences Rhonda Dailey, M.D.; and an investigator development core, led by WSU Department of Internal Medicine Professor and Chair Safwan Badr, M.D.
WSU will serve as the ACHIEVE GREATER coordinating center. Decision-making will be guided by an executive committee consisting of Dr. Levy, each core leader and each project principal investigator.
Stakeholder advisory boards will be included in Detroit and Cleveland.
The support that Dr. Levy and team received from the legislative community, including the Detroit caucus and Black caucus in Lansing, was instrumental. “Without their endorsement, I’m not sure we would have received this grant,” he said.
“Our three integrated research projects all focus on interventions aimed at improving lifespan equality in Black patients by altering the trajectory of heart disease risk using improved access to care and precision tools for personalized health,” Dr. Levy said.

Both Detroit-based projects will leverage the Wayne Health Mobile Unit program to enhance access, layering the planned research on top of usual activities which include daily deployment into different neighborhoods with the specific purpose of screening and population health support. In Cleveland, researchers have teamed with the Cuyahoga Metropolitan Housing Authority, the first chartered public housing authority in the country. CMHA has 60 developments with 10,000 housing units and provides quality, safe, affordable housing to 55,000 low-income individuals and families.
“Deploying resources into Black communities rather than waiting for patients to present to a health care facility is a key component of the lifespan equity lens we will apply across all projects in ACHIEVE GREATER,” Dr. Levy said.
Developed by Dr. Levy in April 2020 to bring COVID testing into hard hit areas, the Wayne Health Mobile Unit program has grown steadily to include vaccinations, preventive services, linkage to social services, as well as hypertension, diabetes and lipid testing, at no cost to patients. The program is funded by the Michigan Department of Health and Human Services through 2024, with additional support from philanthropy and fee-for-service activity.
To date, more than 45,000 people have been served by the mobile units at more than 650 events, with more than 250 different community partners. Since November 2020, more than 2,300 people have received social service assistance at a mobile health unit event, 40% of whom required assistance with public benefits or unemployment; 35% required food assistance and 12% needed help with health insurance navigation or utility bills.

“I am delighted but not surprised that the National Institute of Minority Health and Health Disparities chose Wayne State University to create a Center for Multiple Chronic Diseases Associated with Health Disparities: Prevention, Treatment, and Management. This has been a strong focus for the university, and for me personally throughout my career,” said WSU President M. Roy Wilson. “We have seen in Michigan how focused effort can eliminate health disparities, as it did with COVID-19. We look forward to continuing this life-saving work.”
ACHIEVE GREATER is closely aligned with WSU’s Center for Urban Responses to Environmental Stressors, an NIH-funded P30 led by Professor of Environmental Health Sciences and of Pharmacology Melissa Runge-Morris, M.D., and Case Western Reserve University’s P30 on cancer disparities led by Nathan Berger, M.D., director of the Center for Science, Health and Society.
The grant number for this National Institutes of Health study is P50MD017351.