The Wayne State University School of Medicine has enrolled Michigan’s first patient in a national Phase I/II clinical trial testing whether the implantation of gabanergic interneurons derived from stem cells into the brain of epileptic patients can decrease the frequency of seizures.
The patient had the procedure Nov. 6.
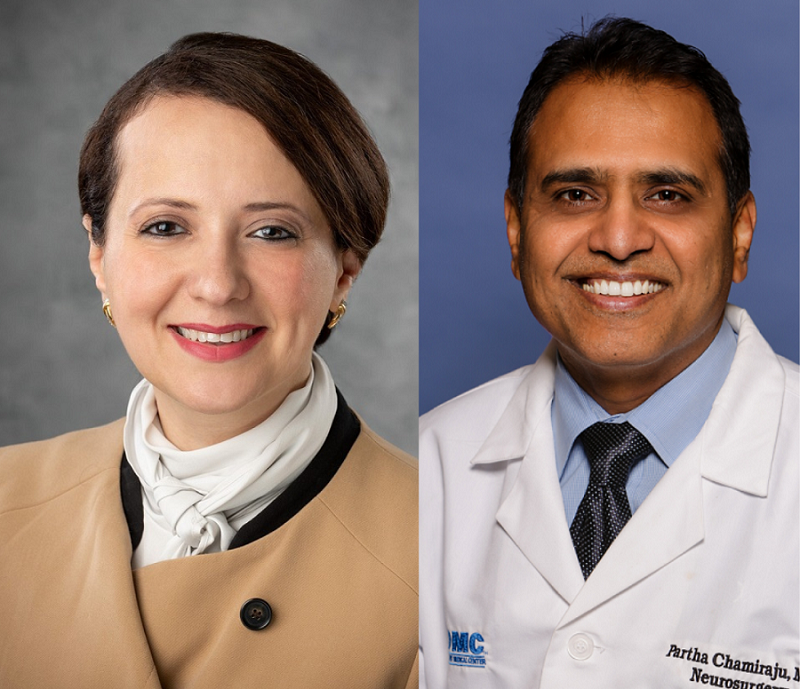
Department of Neurology Associate Professor and Chair Maysaa Basha, M.D., FAES, FANA, is the principal investigator for the Wayne State-based “A First-In-Human Study of Inhibitory Interneurons (NRTX- 1001) in Drug-Resistant Unilateral Mesial Temporal Lobe Epilepsy (MTLE).” She also is chief of the department’s division of Epilepsy.
“Patients who qualify for this study and other types of approved surgeries are considered to have drug-resistant epilepsy. Their quality of life is negatively impacted due to associated psychiatric and cognitive impairment,” Dr. Basha said. “They also have social factors impacting them because seizures limit their ability to drive and sometimes to continue to work. They can be socially isolated due to recurrent seizures.”
Patient No. 14 across the 22 trial locations had the procedure performed by neurosurgeon Parthasarathi Chamiraju, M.D., a clinical associate professor of Neurosurgery.
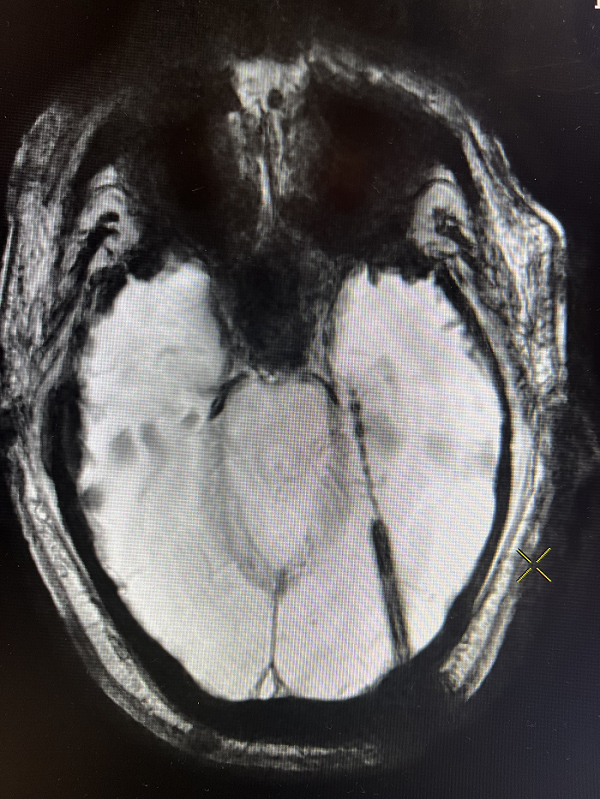
The six-hour procedure uses advanced robotic and stereotactic techniques to create a burr hole in the skull. A probe is then inserted in the hippocampus, the area of the brain assessed to be producing seizures. Guided by magnetic resonance imaging, the specialized cells, which secrete the inhibitory neurotransmitter gamma-aminobutyric acid, or GAGA, are deposited at two-centimeter intervals, with about 10 cell deposits along the hippocampus.
The goal of phase is to assess any serious adverse effects.
“A secondary outcome will be a change (decrease) in seizure frequency in those patients that receive NRTX-1001 compared to baseline and later on compared to those who receive sham treatment,” Dr. Basha added.
In the initial stage, success will be measured by the safety of the procedure and later by observed decline in seizure frequency. Responders will be considered those who end up with 75% reduction of seizures from the baseline.
An estimated 40 patients will then take a drug for one year to partially suppress their immune system to prevent the body from rejecting the cells. Safety, tolerability, evidence of neural cell viability and local inflammation, and effects on epilepsy disease symptoms will be assessed for two years post-transplant. Patients will be followed for an additional 13 years, with quarterly phone contact and annual visits.
For more information on the study, including enrollment criteria, visit FIH Study of NRTX-1001 Neural Cell Therapy in Drug-Resistant Unilateral Mesial Temporal Lobe Epilepsy.