Researchers from the Department of Ophthalmology, Visual and Anatomical Sciences at the Wayne State University School of Medicine have identified three non-antibiotic drugs can protect the eye from severe inflammation during bacterial infection. The drugs can also be used as adjunct therapy with standard antibiotics to minimize infection outcomes.
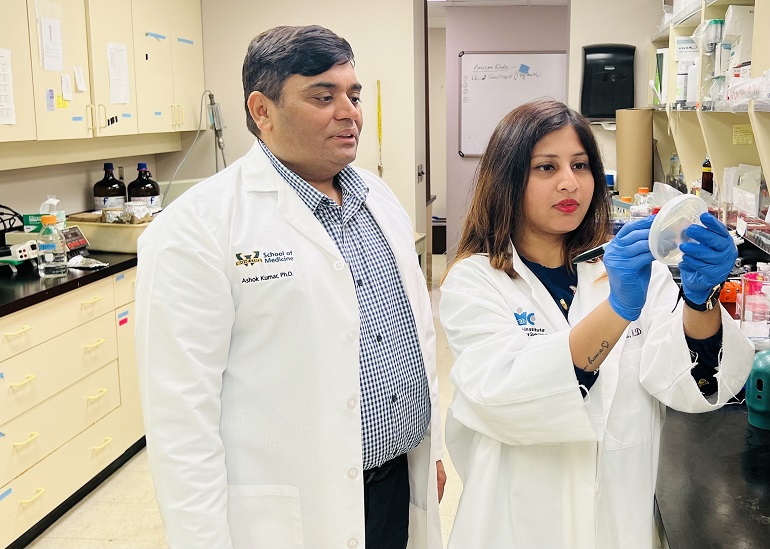
The study was led by Ashok Kumar, Ph.D., an associate professor of Ophthalmology, Visual and Anatomical Sciences and a principal investigator at Kresge Eye Institute. His laboratory has been involved in investigating host pathogen interactions and new treatment options in bacterial, viral and fungal eye infection models for several years.
“One of the ways to identify new drugs for any disease includes drug repurposing, where we can identify additional uses for already-approved drugs, enabling the quickest and cheapest possible transition from bench to bedside,” Dr. Kumar said.
Susmita Das, Ph.D., a postdoctoral fellow in Dr. Kumar’s laboratory, is the lead author on “Transcriptomics and systems biology identify non-antibiotic drugs for the treatment of ocular bacterial infection,” published in iScience, a Cell Press journal.
Post-operative ocular infections are a major concern among ophthalmologists, as it could lead to potential blindness if not treated promptly. One of the most common infections after eye surgeries is Staphylococcus aureus-induced endophthalmitis, in which bacteria from the outside gains access to the inner eye.
“The current management of this complication involves local or systemic antibiotic therapy, which efficiently kills the microbe but does little to reduce inflammation,” Dr. Kumar said. “But, around 50% of these infections are also caused by different antibiotic-resistant strains of the bacteria, which predispose the patients to treatment failure and vision loss.”
In their search for alternative therapeutics to treat ocular infections, they used high-throughput techniques of transcriptomics to understand the genome-level alterations involved in the host response during bacterial endophthalmitis, and adopted an innovative systems biology approach to identify key molecules and pathways associated with Staphylococcus aureus endophthalmitis, Dr. Das added.
Working with study collaborator Manoj Bhasin, Ph.D., of Emory University in Atlanta, Ga., who performed in-silico studies, including CMap analyses, the team predicted the three drugs that reversed gene signatures of bacterial endophthalmitis in an animal model’s retina -- Dequalinium chloride, Clofilium tosylate and Glybenclamide.
The study team tested the efficacy of the drugs and revealed that all exhibited anti-inflammatory properties against both antibiotic-sensitive and resistant bacterial strains in human cultured retinal cells.
“We were excited to find that, while intravitreal injections of all the drugs reduced intraocular inflammation in even methicillin-resistant SA-infected mouse eyes, DC and CT were able to reduce bacterial burden too. Drug treatments improved visual function and protected the eye from retinal cell death,” Dr. Das said.
“We also wanted to check the outcome of the disease following an adjunct therapy of these drugs with the existing antibiotic treatment during ocular infection and found that these drugs demonstrated synergy with vancomycin in improving disease severity,” Dr. Kumar said. “We are currently investigating the mechanisms underlying antimicrobial and anti-inflammatory properties of these drugs and testing their efficacy against other bacterial pathogens in order to fully elucidate the crosstalk between the drugs, the host and the microbe.”
The work was supported by National Institutes of Health grants to Dr. Kumar (R21AI135583, R01EY026964 and R01EY027381).