Scientists in the Department of Ophthalmology, Visual and Anatomical Sciences at the Wayne State University School of Medicine have revealed that COVID-19 patients might harbor the virus in their eyes, demanding screening of ocular tissues before transplant surgeries during the pandemic.
Sneha Singh, Ph.D., a postdoctoral fellow in the laboratory of Associate Professor Ashok Kumar, Ph.D., and Eversight Director of Research Onkar Sawant, Ph.D., co-led the study, Prevalence of SARS-CoV-2 in human post-mortem ocular tissues, presented Nov. 7 at the 2020 Cornea and Eye Banking Forum and published in The Ocular Surface.
The study was conducted in collaboration with Eversight, which provided the researchers COVID-19 patient donor ocular tissue for the research.
Dr. Kumar was one of two corresponding authors for the study. The ongoing investigation has been supported by the Eye Bank Association of America, the National Eye Institute, and the National Institute of Allergy and Infectious Disease. Findings underscore the critical importance of eye donor screening guidelines, postmortem nasopharyngeal PCR testing for detecting the virus and appropriate disinfection at the time of tissue recovery to mitigate the risk of transmission through eye tissue donation and transplantation.
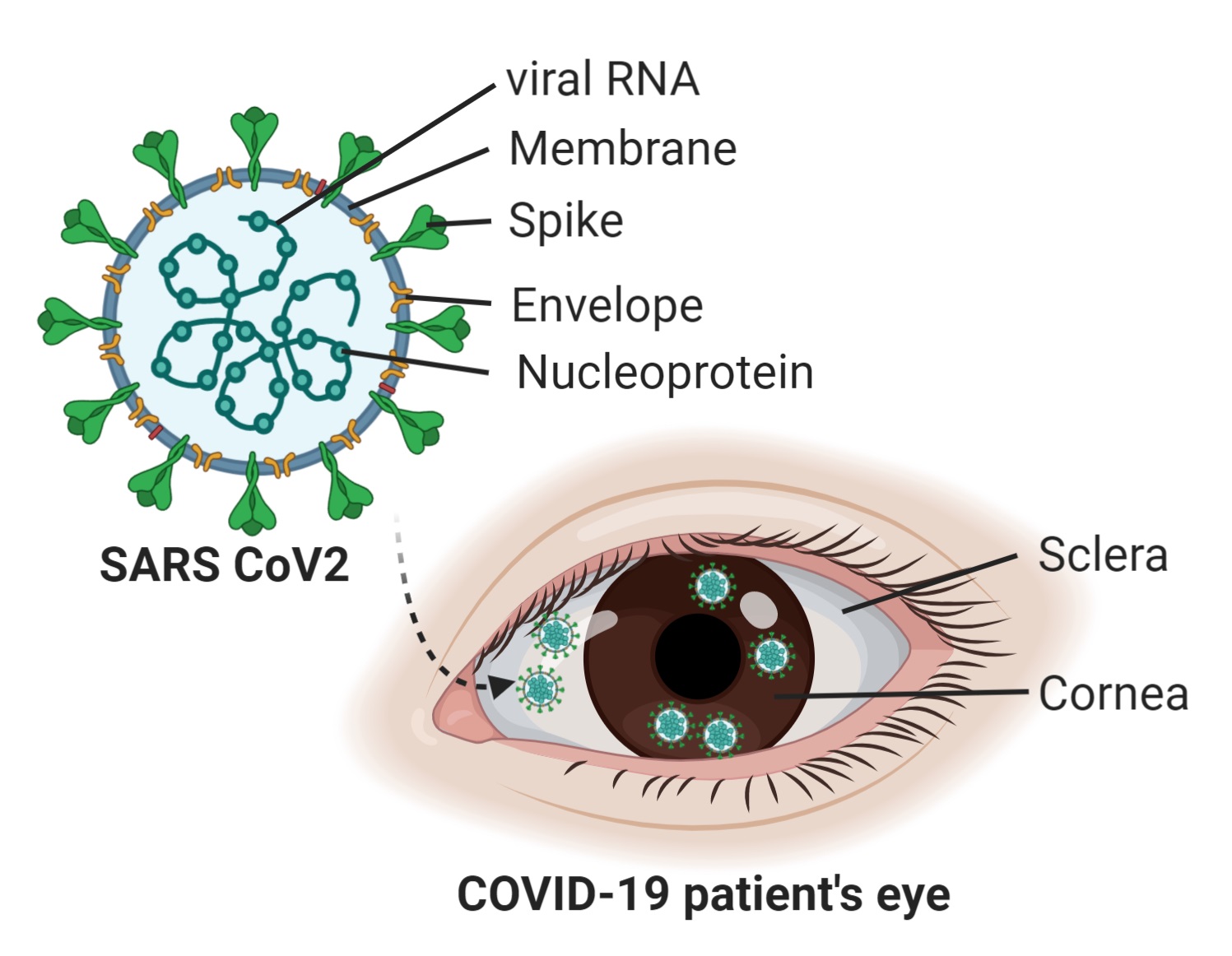
Severe acute respiratory syndrome coronavirus 2, SARS CoV-2, first emerged in December 2019, causing the COVID-19 pandemic. The eye may serve as an additional point of entry for the virus and lead to the spread of infection. The speculations caused alarm for eye donor organizations, leading them to screen cornea tissue before acceptance for transplant surgeries.
Eversight is a nonprofit organization with a mission to restore sight and prevent blindness through donation, transplantation and research. The Eversight network is responsible for recovering, evaluating and providing human eye tissue for transplantation; supporting research into the causes and cures of blinding eye conditions; promoting donation awareness through public and professional education; and providing humanitarian aid to people around the world in need of corneal transplantation.
“The slightest possibility of the virus being harbored in the eye as a transmission or infection route is alarming,” Dr. Kumar said. “There are a few reports on the effect of virus infection in the cornea, as well as the retina, causing minor complications. Therefore, we decided to collaborate with Eversight and screened more than 150 donor eye tissues for the presence of the SARS CoV-2 virus and provided evidence to rule out the infected tissues from transplant surgery.”
His laboratory has focused on studying the host-virus interaction with ribonucleic acid viruses, including studying the ocular pathology during the Zika virus epidemic as well.
“We had shown the capability of the virus to infect the eyes and developed an animal model to study the disease pathology in the eye. In our studies, we had also shown that ZIKV was capable of infecting the corneal cells as well as the retinal pigment epithelial cells, and caused chorioretinal atrophy, leading to compromised vision,” he added.
In addition to WSU and Eversight researchers, the study team included University of Michigan researchers, led by Professor Shazad Mian, M.D., and Chicago’s Rush University, led by Associate Professor Parag Majumdar, M.D.
The presence of the SARS CoV-2 virus receptors on the outer surface of the eye makes it a suitable candidate to be infected by the virus upon exposure and can lead to transmission and spread of the virus in the body.
The researchers screened samples comprised of cornea, sclera and iris from COVID-19-positive donors.
“We could detect the presence of viral Spike and Envelope protein in the cornea of the COVID-19 positive donor tissues. These pieces of evidence indicate that the virus is capable of infecting the corneal tissue,” Dr. Singh said.
Several questions remain.
“Our findings show that the virus is capable of infecting the cornea, but we still don’t know if it can replicate and transmit to the other tissues in the eye, thereby causing a spread of the virus,” Dr. Kumar said. “Therefore, we are planning to further confirm our observations with advanced techniques of fluorescent in situ hybridization to detect the replication of the virus in the tissues. We are currently screening more tissues for the virus presence as there has been a resurgence in the COVID-19 cases in the U.S. We plan to study the transmission of the virus using human corneal explant tissues and primary human corneal epithelial cells. We are highly interested to understand the innate immune response to SARS-CoV-2 in corneal tissue, which will lead to a better understanding of the disease pathology.”
The research and clinical findings are in the early stages, and require investigation to understand the disease pathology and future complications to patients exposed to the virus, he added.
“As evidenced by the Zika virus epidemic, the infants from infected mothers had complications in their vision months after exposure to the virus,” Dr. Kumar said. “COVID-19 patients might experience eye-related complaints post-recovery from the infection. Therefore, we do not need to panic, but stay alarmed and take all the necessary precautions to contain the exposure to the virus and pursue active research to understand the disease pathology and its future implications on mankind.”