Why are newborns born to mothers with COVID-19 rarely infected? Researchers at the Wayne State University School of Medicine and the Perinatology Research Branch of National Institute of Child Health and Human Development/National Institutes of Health in Detroit have found that placental cells minimally express the instructions, or mRNA, to generate the cell entry receptor and protease required by the virus that causes COVID-19 to invade human cells.
The pandemic caused by SARS-CoV-2 has infected more than 10 million people worldwide, including pregnant women, yet to date there is no consistent evidence that pregnant mothers pass the virus to their newborns.
While pregnant women represent a potential high-risk population given that other viral infections such as Zika, cytomegalovirus and rubella can be passed from mother to fetus, the evidence for vertical transmission of SARS-CoV-2 is rare, and acquisition of the virus in the nursery cannot be excluded.
A requirement for a virus to infect a cell is that cell surface expresses a receptor for the virus. The main receptor for the new coronavirus is the angiotensin converting enzyme 2, or ACE2. The spike protein of the virus – the spikes seen in the images of the virus – is activated by an enzyme called TMPRSS2. Cells that co-express ACE2 and TMPRSS2 such as those found in the lungs are particularly vulnerable to infection.
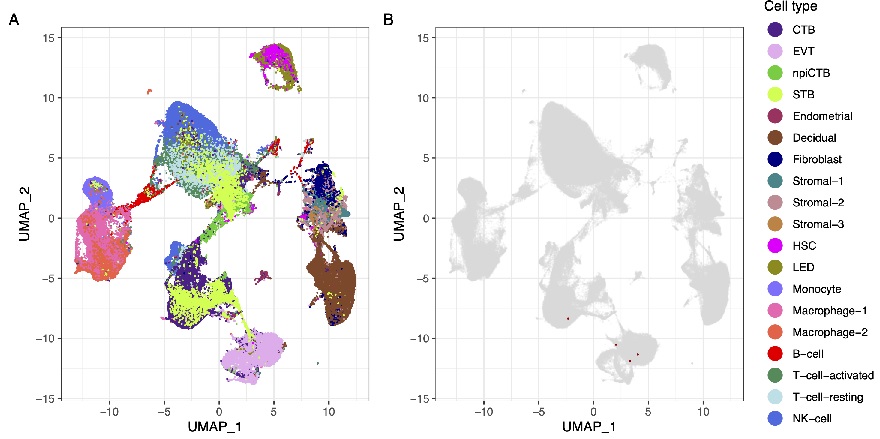
In the study “Does the human placenta express the canonical cell entry mediators for SARS-CoV-2?”, published today in the journal eLife, WSU and PRB researchers employed cutting-edge molecular techniques such as single-cell genomics to determine whether human placental cells express the mRNA for the mediators that the virus SARS-CoV-2 uses for entry into the cell. The researchers concluded that placental cells do not express the transcripts needed to develop the receptors that the virus requires to facilitate vertical transmission from mother to the fetus.
“The findings of this study help to understand why mother-to-fetus transmission is so rare (less than 2% of cases),” said Roberto Romero, M.D., D.Med.Sci, chief of the PRB. “The most likely explanation is that the cellular instructions for the production of the main receptor for SARS-CoV-2 are not expressed in the human placenta. In contrast, the receptors for other viruses known to cause fetal infection such as Zika and cytomegalovirus were found in placental cells.”
Roger Pique-Regi, Ph.D., assistant professor of the WSU Center for Molecular Medicine and Genetics, and of Obstetrics and Gynecology, first author of the study, explained that the single-cell genomics technology the researchers employed allows them to study the transcriptome of individual cells isolated in tiny oil droplets using microfluidics.
“This allows us to obtain at an unprecedented level of detail the multiple different cell types and the genes being expressed in gestational tissues,” said Dr. Pique-Regi, head of the Single-Cell Genomics Section of the PRB. “Here, we have dissected at the molecular level the different cell types of the human placenta across trimesters, and the membranes enveloping the fetus in the third trimester. This allowed us to determine which cell types are present and if they express the genes necessary for viral infection and spreading.”
While the study allows the possibility that SARS-CoV-2 could infect the placenta via alternate entry routes while interacting with other proteins, the findings provide strong evidence that it is unlikely to infect the placenta and fetus through the traditional cell entry mediators.
“Single-cell and single-nucleus RNA sequencing allowed us to investigate the expression of the main cell entry mediators for SARS-CoV-2 by the human placenta throughout pregnancy,” said Nardhy Gomez-Lopez, Ph.D., associate professor of the WSU Department of Obstetrics and Gynecology and head of the Immunobiology Section of the PRB. “Our findings revealed that the human placenta lacks expression of such mediators, providing an explanation for the paucity of vertical transmission in pregnant women with COVID-19. Yet, placental cells do express the receptors for other viruses such as Zika, cytomegalovirus and rubella, explaining why some infections affect the fetus and others are unlikely to do so.”
Other members of the research team include Adi Tarca, Ph.D., professor of WSU Obstetrics and the Gynecology, Bioinformatics and Computational Biology Unit of the WSU School of Medicine Perinatal Initiative; Francesca Luca, Ph.D., associate professor of WSU Molecular Medicine and Genetics, and of Obstetrics and Gynecology; Yi Xu, PRB research associate; Adnan Alazizi, Center for Molecular Medicine and Genetics researcher; Yaozhu Leng, PRB research assistant; and Chaur-Dong Hsu, M.D., chair and Frank P. Iacobell Professor of WSU Obstetrics and Gynecology.
A video of the study is available here.