Students and faculty from Wayne State University’s School of Medicine and Eugene Applebaum College of Pharmacy and Health Sciences hosted 33 Michigan veterans of the U.S. Air Force, Army and Marines during the course of three sessions June 6, 13 and 20 to better understand the health needs of veterans. The veterans served in the Vietnam and Gulf Wars.
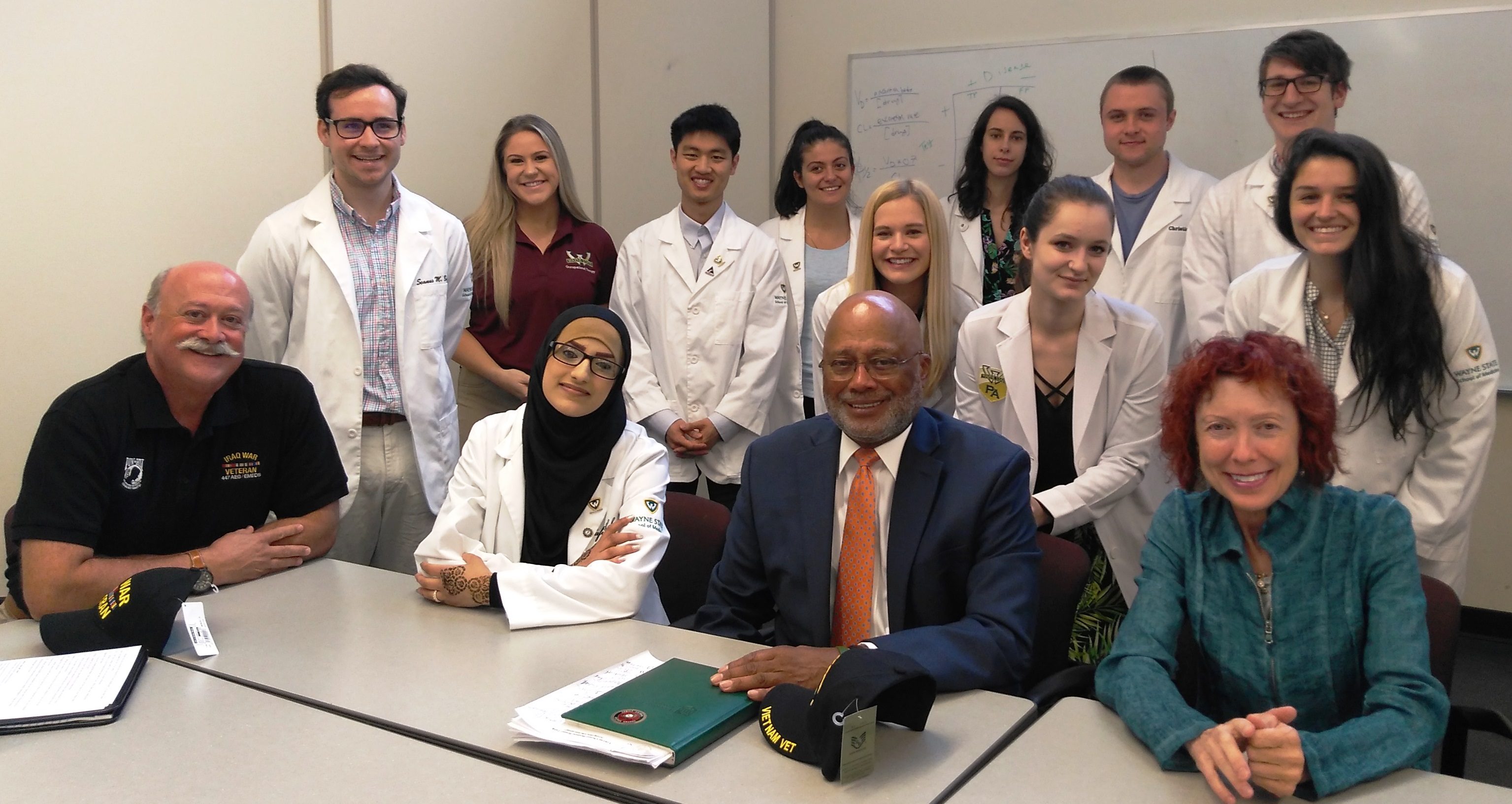
The goal of the sessions, held in the School of Medicine’s Scott Hall and the Richard J. Mazurek, M.D., Medical Education Commons, was to ensure students continue to understand the social and economic impacts of health care on veterans.
The June 6 visit coincided with the 75th anniversary of D-Day, the Allied invasion of Normandy, and the start of the 2018 Mission Act granting veterans the option of seeking care in the private health care sector when the wait at a Veterans Affairs facility is too lengthy.
The veterans trained 375 medical students, pharmacy students, physician assistant students, social work and occupational therapy students June 20 as part of the medical school’s Population, Patient, Physician and Professionalism Course, or P4.
“As a student, this experience has been invaluable in that I didn't have to use the internet to imagine what my future allied health colleagues would do; I could ask them directly and get a better understanding from their own, unique perspectives,” said Class of 2022 medical student Joshua George-Lopez. “It assured me that I don't have to be alone in my decision-making when it comes to making a plan for my future patients, which was oddly a relief to a stressor I hadn't yet thought about.”
An interprofessional staffed helped to facilitate the curriculum.
“Students learned to recognize, reflect upon and discuss the importance of eliciting a military health history in order to identify selected health, mental health and psychosocial challenges experienced by veterans transitioning from military to civilian life,” said Associate Professor of Pediatrics Nakia Allen, M.D., F.A.A.P., who directs the course.
P4 is a Year 1 to Year 2 course that emphasizes the evolving professional identity of a physician connected to patients and populations. The course exposes students to their roles as clinician, leader, interprofessional collaborator, scholar and systems analyst through large-group sessions, small-group sessions, online modules, self-directed reflective assignments and clinical opportunities in the community.
The veterans health session took an interdisciplinary approach to learning about a core group of health care constituents.
“This was our first time participating in the Veterans Health curriculum, and we are so incredibly thankful our students were awarded the possibility. We had 48 of our first-year students participate in the three-week course and the response was overwhelmingly positive. We felt this was an excellent opportunity to learn about the community we serve and grow our cultural competency while simultaneously learning about each others’ professions,” said Corinne Gratson, M.S., P.A.-C., an instructor in the College of Pharmacy and Health Sciences Physician Assistant Studies Program.
The meetings included panels, case conferences and interprofessional activities.
They also learned best practices in the clinical assessment, treatment and care of veterans with musculoskeletal injuries and neuropathies related to vibration injuries; conducted biopsychosocial assessments; and learned to work collaboratively with physical and mental health professionals in developing treatment and care plans for veterans, military service members and their families.
The veterans also helped the students understand stigma, ways to foster resilience and shared resources to help veterans access health and behavioral health services and reintegrate more successfully into communities.
“One other thing that stood out to me in this unit was how little I previously knew about the distinct health care required to best serve veterans, and this is coming from someone with a background involving the military and VA,” George-Lopez said. “Between veteran specific histories and a fresh set of community resources, I am very grateful for the new skills this P4 curriculum has given me for my physician toolkit.”
Gratson’s students also had minimal prior knowledge of veterans, veterans’ health, the VA and the military.
“Not only did this provide an opportunity for our students and faculty to learn about a very important portion of our patient population and the special health issues they face, it also afforded us a way to collaborate with other professionals in an effort to provide our veteran patients with the best, most comprehensive care possible,” she said. “It was great to see our students taking an active role in helping identify possible health issues, both mental and physical, as well as helping to coordinate care. Understanding and learning how to care for the long-term effects of military life makes us better providers for those men and women who have served.”
The unit was made possible with help from NorthStar Care Community Chief Medical Officer Michael Paletta, M.D., who provided opening and closing lectures on military culture. Dr. Paletta is an assistant professor of Family Medicine and Palliative Medicine at WSU, and a 1983 graduate of the medical school.
The P4 Course for the Class of 2022 began in the summer of 2018 with a poverty simulation exercise, followed by a unit on aging and falls prevention in January and a unit on food insecurities last month, all from a hands-on, clinical-based perspective.