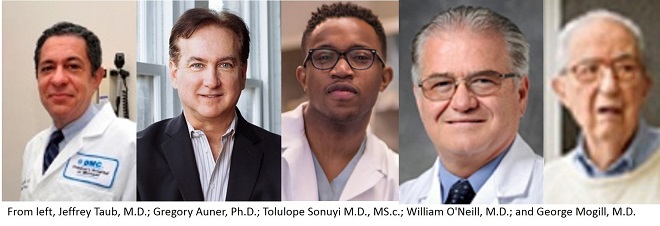
Five of Crainâs Detroit Businessâ 2018 Health Care Heroes are connected with the Wayne State University School of Medicine, either as faculty or alumni.
Jeffrey Taub, M.D., professor of Pediatrics and endowed chair in pediatric cancer research for the Wayne State University School of Medicine, won in the Oncology Research Category.
A cancer survivor himself, Dr. Taub has been treating cancer for 30 years at Childrenâs Hospital of Michigan.
He led the largest study on survival outcomes for children with Down Syndrome who also develop acute lymphoblastic leukemia and acute myeloid leukemia, a study that led to new tests and treatment protocols for these children.
Children with Down syndrome have a 10 percent to 20 percent increased risk of developing acute lymphocytic leukemia and acute myeloid leukemia compared to children without Down syndrome. They are considered to have one of the highest risks of developing leukemia and require focused treatment protocols that differ from those for children with the syndrome.
Dr. Taubâs study, âImproved outcomes for myeloid leukemia of Down syndrome: A report from the Childrenâs Oncology Group AAML0431 trial,â published in the June 2017 edition of Blood, a weekly medical journal published by the American Society of Hematology, enrolled 204 children from 2007 to 2011 through the Childrenâs Oncology Group, an international organization that links all major pediatric oncology centers in the United States, Canada and other countries to develop treatments for children with cancer.
Dr. Taub said children with Down syndrome and AML or ALL have special needs, and there have been concerns that they suffer more side effects from treatments compared to children without Down syndrome. These children require treatment protocols that focus on their clinical needs to provide effective and safe treatments. Children with Down syndrome represent 15 percent of all pediatric AML cases, which is significant as they represent about one in 800 children in the general population.
The study showed that the overall cure rate of Down syndrome patients was 93 percent, while deaths from side effects were very low. The most common side effects experienced by patients were infections that occurred when their white blood cell counts were low. No children died due to cardiac complications that had been reported previously (44 percent of children in the study had congenital heart defects).
An important part of the study also addressed the assessment of a test known as minimal residual disease, or MRD, monitoring. The test can detect one leukemia cell amongst 10,000 normal blood cells in the bone marrow. This is a more sensitive and accurate way of detecting leukemia cells compared to the standard approach of looking at bone marrow slides under a microscope. Patients who had a MRD level of less than .01 percent after the first course of chemotherapy experienced exceptionally high cure rates. Patients who had detectable MRD rates of greater than .01 percent had worse outcomes.
This is the first time that a laboratory test can potentially identify how children with Down syndrome and AML will respond to chemotherapy (this has been used previously for children without Down syndrome and AML). Patients with a negative MRD test had cure rates of 92.7 percent compared to 76.2 percent for patients with a positive test.
Read the article here.
Gregory Auner, Ph.D., professor of Surgery for the School of Medicine, won the Health Services Research Category.
Founder and chief science officer of Seraph Biosciences Inc., a company based on technology licensed from Wayne State University, Dr. Aunerâs research has led to the development of the Seraspec, a portable, point-of-care device that can offer real-time pathogen detection and identification in patients.
The Seraspec utilizes proprietary micro sensors to enable the technology of Raman Spectroscopy to molecularly analyze pathogens. The technology can generate a âmolecular fingerprint,â allowing for nearly immediate identification between antibiotic-resistant and non-antibiotic resistant pathogens.
The patented technology, according to the company, eliminates the need for time-consuming and costly laboratory-based methods of specimen collection, processing and identification.
Current devices incorporating Raman Spectroscopy are the size of a table, limiting their portability and use in the field. Samples from patients must be cultured for several days, growing enough pathogens for an identification. The Seraspec is the size of a small suitcase â" and Dr. Auner is working to make the device even smaller â" and can identify pathogens in 100 milliseconds.
Dr. Auner, the Strauss Endowed Chair and professor of the Department of Surgery and Biomedical Engineering, is also the founder and director of the Smart Sensors and Integrated Microsystems Program. He has been appointed to the National Academies Board on Manufacturing and Engineering Design, has written more than 250 publications and has more than 30 patents (issued and pending).
Read the article here.
Tolulope Sonuyi M.D., MS.c., clinical assistant professor of Emergency Medicine and an emergency physician at DMC Sinai-Grace Hospital, won in the Physician category.
He was selected for his founding of DLIVE, the first hospital-based violence intervention program in Michigan. He worked with My Brother's Keeper, to create in 2016 DLIVE, or Detroit Life Is Valuable Everyday, which is based in Sinai Grace Hospital with the Wayne State University Department of Emergency Medicine.
DLIVE works with youth and young adults who have sustained acute intentional violent trauma to eradicate the future morbidity and mortality predicted by the initial injury, prevent retaliatory violence, prevent incarceration often associated with individuals who have been victims of traumatic violence and to facilitate a pathway toward success and prosperity.
Dr. Sonuyi coordinates a multi-disciplinary team of doctors, nurses, social workers, mental health specialists, violence intervention specialists and volunteers assist victims of violent trauma to adopt their injury as a springboard to change their lives. Trained violence intervention specialists provide crisis intervention, trust-building, engagement, mentorship and linkage between the hospital and Detroit community support so that trauma patients are involved in an evidence-based strategy for success when they are discharged from the hospital.
Read the article here.
William O'Neill, M.D., a 1977 graduate of the School of Medicine, won in the Heart and Vascular Research category for his leadership is interventional cardiology.
Dr. OâNeill completed a residency at the WSU School of Medicine and a fellowship at the University of Michigan Hospital. He continued at UM, becoming director of the Cardiac Catheterization Laboratory and associate professor of Medicine, before joining William Beaumont Hospital as director of the Division of Cardiovascular Medicine.
In 2006, he left Michigan for the University of Miami Miller School of Medicine as executive dean for Research, Research Training and Innovative Medicine, and later as chief executive officer for Research.
In 2012, he returned to Detroit, joining Henry Ford Hospital as medical director of its new Center for Structural Heart Disease, focusing on new minimally invasive treatments for heart failure and heart valve disease.
Dr. OâNeill cowrote the first randomized trial of intracoronary streptokinase therapy for acute myocardial infarction, and initiated the first randomized trial of balloon angioplasty. He also pioneered balloon valvuloplasty for aortic and mitral stenosis, and outpatient angioplasty, and was involved in the largest international interventional study ever to develop a new oral glycoprotein IIb/IIIa antagonist.
He was a founding member of the American Board of Internal Medicineâs Interventional Cardiology Board, which certifies all interventional cardiologists, and the founding chair of the Innovation in Intervention Summit of the American College of Cardiology. He has served on the American Board of Internal Medicine Subspecialty Board of Interventional Cardiology and the Scientific Program Committee of the American College of Cardiology.
He is the author of more than 300 hundred peer-reviewed articles and abstracts, has written multiple book chapters, and edited one of the first textbooks in the field of interventional cardiology.
Read the article here.
George Mogill, M.D., a 1942 graduate of the School of Medicine, was a co-winner of the Lifetime Achievement category.
Dr. Mogill is a retired Family Medicine physician. He received his bachelorâs degree in biological sciences from WSU in 1937. He graduated from the Wayne University College of Medicine in 1942, completed a one-year surgery internship, and then joined the United States Army Medical Corps in 1943. He landed in Normandy four days after D-Day, caring for patients in the Armyâs 8th Field Hospital in France and Germany. He moved home to complete his residency when the war ended.
He opened his Detroit office on Second Avenue between Peterboro and Charlotte streets, near the Masonic Temple, and rounded at Grace in the morning and at lunch, seeing 30 to 40 patients a day. His mother was the office nurse. He also visited homebound patients referred by the Wayne County Medical Society.
He moved his practice to Royal Oak for a time before returning to a WSU-affiliated medical school clinic to secure the schoolâs Family Medicine residency. He joined the School of Medicineâs faculty in 1972 as a clinical instructor in the Department of Family Medicine.
He continued to teach throughout the 1990s and into the 21st century.
Dr. Mogill was chief of the Department of Family Practice at Harper-Grace Hospital from 1977 to 1984 and later at Sinai-Grace Hospital. He was named an honored alumnus of the Alpha Omega Alpha Medical Fraternity in 1980. He received the Southeast Michigan Quality of Care Award presented by Pfizer Inc., in 2000. In 2006, he received both the Exemplary Teaching Award from the American Academy of Family Physicians and the Lifetime Achievement Award from the Michigan Academy of Family Physicians.
He is a lifetime member and former board member of the School of Medicine Alumni Association. In addition, the George Mogill, M.D., Endowed Award for Family Medicine â" a gift to the school established in 2000 by a former patient of the doctor â" is presented annually during Match Day to a graduating senior committed to specializing in Family Medicine. The award is based on qualities and characteristics exemplified by Dr. Mogill, including scholastic achievement, compassion, volunteerism, leadership, respect of peers, and a sense of humor and joyfulness.
Read the article here.