Three faculty members in the Wayne State University School of Medicine Department of Family Medicine and Public Health Sciences collaborated with a national consortium to identify strategies for successfully recruiting and retaining diverse ethnic communities in practice-based research.
"A consistent and overarching theme that emerged was the importance of viewing the research process as interrelated and continuous across time and studies," said study principal investigator and WSU Professor Victoria Neale, Ph.D., M.P.H. "We were able to cull a general set of seven strategies constituting the four research stages across racial/ethnic groups; however most of these general strategies were expressed differently for each racial/ethnic group based on distinct social contexts, cultural variations and life experiences."
The study involved interviews with 24 practice-based researchers and focus groups with 172 patients from African-American, Arab and Chaldean, Chinese, Hispanic and Navaho communities. WSU's Dr. Neale, Assistant Professor Kimberly Campbell Voytal, Ph.D., M.S.N., and Professor and Assistant Dean of Clinical Education Kendra Schwartz, M.D., M.S.P.H., co-led the portion focusing on Arabic-, Chaldean- and English-speaking individuals with Arab or Chaldean ethnicity.
"Representative participation in research is necessary for successful implementation of innovation into community-based practices that serve minority, underserved and vulnerable groups," Dr. Neale said. "An important step to reduce health disparities is to understand how to integrate diverse populations and the clinicians who provide their care into practice-based research. Greater participation of minority and underrepresented patients in clinical research is recognized as vital to reducing avoidable morbidity and mortality from common health conditions."
The results were published in the November/December 2013 issue of Annals of Family Medicine, and can be accessed at http://annfammed.org/content/11/6/550.
Dr. Neale was responsible for coordinating the achievement of the specific aims at each participating site.
Primary Care Multi Ethnic Network is a consortium of practice-based research networks with a common interest in improving the health of underserved and vulnerable populations. Sites included Detroit (called MetroNet in the network); Dayton, Ohio; San Francisco; Houston; and New Mexico.
For the MetroNet portion, the WSU team interviewed researchers experienced with working with the Arab and Chaldean community, asking about strategies for recruiting and retaining members of these groups into clinical research studies. They used the findings to develop a focus group discussion guide and then standardized the guide for use across the five networks with a common set of questions. Networks made minor adjustments to customize the guide to their specific populations.
The team then held four focus groups, in English and the participants' native language, at a service provider in Dearborn and at local churches. Focus group participants advised that researchers must build trust with community and clinical partners before study implementation. "If someone were to come out into the community … and we don't know them, but they wanted to ask us some questions, we probably wouldn't be able to be open to them, because … we'd be unsure of them," one participant told the study administrators.
A researcher interviewed here - called a key informant in the study - said the stigma around topics such as mental health, suicide, divorce, rape, AIDS/HIV and sexuality are "very hush-hush things. It requires a skilled, respected and trusted communicator to address these issues."
"Both sets of participants - key informants and focus group members - identified common elements believed to influence success in the recruitment and retention of racial/ethnic minority populations in research studies," Dr. Neale added.
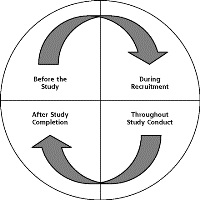
The study authors used the interview results to build a four-stage "Cycle of Trust" model for developing and sustaining relationships.
The PRIME Net Center is funded by the NIH National Center for Minority Health and Health Disparities. The affiliates will now develop activities with their member practices to launch studies that address concerns of underserved and vulnerable patients.